
Critical Access Hospitals provide healthcare to rural communities, many of which are considered medically underserved. Fewer people are living in rural areas of the US and this low population density correlates with higher numbers of uninsured or underinsured patients. There are over 1,300 Critical Access Hospitals in the US and they serve as a lifeline for more than 40 million patients in the US. Critical Access Hospitals are unique due to a combination of factors. The Centers for Medicare and Medicaid Services (CMS) requires that facilities designated as Critical Access Hospitals are small, with less than 25 acute care inpatient hospital beds. They also must offer 24-hour emergency department services and typically have a relatively short Length of Stay, with an average LOS under 96 hours. Additionally, Critical Access Hospitals are typically more than 35 miles from the closest hospital (or 15 miles from the closest hospital where there is mountainous terrain or only secondary roads).
The COVID-19 pandemic hit Critical Access Hospitals hard especially in the area of labor shortages and rising costs. To meet the challenge, successful facilities will turn to innovative approaches to bend the curve on labor costs. They will look to technologies that enable nursing staff to practice at the top of their licenses and maximize their scope of practice. This may include use of solutions such as secure chat to enable team-based care or the use of chatbots for patient outreach and education. These tools can reduce the time that staff spends on repetitive tasks, increasing staff satisfaction and improving retention rates.
As part of the requirements for designation as a Critical Access Hospital, facilities must have robust quality management programs. Data is often collected on patient engagement (including discharge information and transitions of care) as well as compliance with recommended immunizations for healthcare personnel (including influenza). Both of these measures can be enhanced through the use of chatbots. For patient engagement, chatbots can deliver key information to patients and help identify those who require additional support.

For staff immunization campaigns, chatbots can be used to communicate with staff who haven’t been vaccinated and allow them to schedule an appointment real-time, without phone calls or having to access online systems.
Data may also be collected on measures related to the management of myocardial infarction. Secure chat can enable rapid, HIPAA-compliant communication among providers to reduce delays in critical patient care processes.
In the decade prior to the pandemic, more than 130 rural hospitals closed. Federal funds released during the pandemic helped stem that tide, but as the declared public health emergency comes to a close, facilities must cope with the loss of that funding lifeline. The Center for Healthcare Quality & Payment Reform estimates that more than 30 percent of rural hospitals are at risk at closing in the next three years due to cost pressures.
One major contributor to rising costs is staff turnover. This can be significant, especially given the challenges of recruiting clinicians to live and practice in rural areas. Understanding staff engagement will be a key priority for successful facilities, and chatbots can be a tool for rapid assessment of staff satisfaction.
In some areas, the Critical Access Hospital is the primary location for the delivery of ambulatory services, such as radiology or laboratory testing. Many patients experienced delayed care during the pandemic. Facilities looking to close these gaps in care while controlling costs can use chatbots to remind patients of the need for preventive services such as mammograms and well-child visits and immunizations rather than sending more costly reminder letters. Organizations have experienced a 27% increase in well-child visits using chatbots providing patient education, anticipatory guidance and easy scheduling.
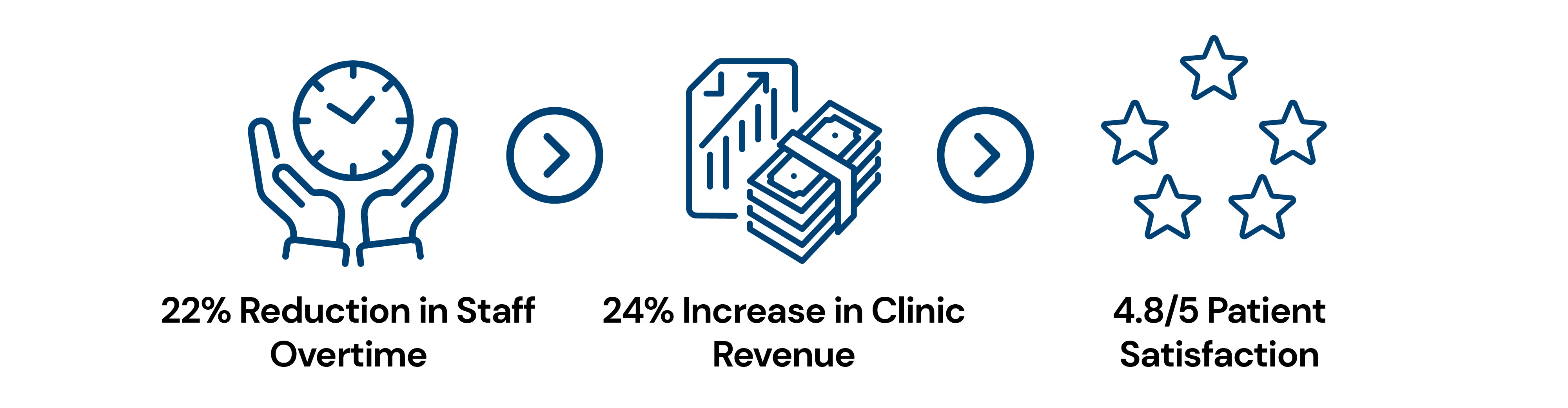
Chatbots can also be used for appointment reminders and allowing patients to easily reschedule appointments when a conflict arises, reducing the burden on scheduling and patient care teams. Chatbots can also eliminate burdens for registration and billing teams, by automating the capture of billing information such as insurance card images or photo IDs. For example, one clinic was able to reduce patient throughput by 19 minutes per patient automating patient intake. This resulted in:
For many years, Critical Access Hospitals have been the backbone of care delivery in the rural US. By embracing innovative solutions and new technologies, they can streamline processes and help conserve resources, continuing to serve their communities for years to come.
