
With the ongoing shift from Fee For Service (FFS) Care to Value-based Care, the need to proactively reach out to patients has gone from nice to have to critical to the financial success of the practice.
Routine care is essential to detect, prevent, and treat illness, yet data shows that only 10% to 25% of patients schedule a needed visit. Since providers rely on these visits to detect and address gaps in care, and manage chronic conditions, managing only patient-initiated visits is unlikely to achieve either Value-based Care or health targets.
Patient portals, which have become increasingly popular in recent years, are secure websites through which patients access personal health information. Patients can:
But even with the convenience and ease of these tools, many adults are not using portal services. About 3 in 5 individuals nationwide reported they were offered and accessed their online medical record or patient portal in 2022. This is an improvement since 2020, yet the most common reason to access the portal is to access their medical record and test results, which is most likely to be AFTER an interaction with their provider. Black and Hispanic individuals were offered and accessed patient portals at significantly lower rates than White individuals.
A nudge is an attempt to influence user behavior by presenting options to them. Nudges help individuals make wiser choices by subtly altering the environments in which those individuals make decisions. Importantly, to qualify as “nudges,” these “choice architecture” strategies do not mandate or forbid options, and they do not meaningfully change the financial incentives associated with various options. Rather, nudges tap into the psychology of decision-making and gently guide individuals to different outcomes. Nudges are perfect for improving participation and commitment to a cause of action. In the two examples below, recipients were encouraged to make an active choice to be seen and then provided a simple way to execute that decision.

AllianceChicago noticed a concerning decline in preventive health visits for children and adolescents. To address this finding, AllianceChicago’s healthcare providers and staff implemented an innovative mechanism to use AI chatbots to engage caregivers in evidence-based preventive care for children. They provided access to Quincy’s conversational chatbots to in-network parents and guardians who are 82 percent racial and ethnic minorities of approximately 10,500 children.
The human-centered digital outreach, which did not require an app, reminded families in their preferred language of upcoming well-child visits and immunizations, provided anticipatory guidance materials from the CDC before the visit to enrich the dialogue, and facilitated easy appointment scheduling of babies and children for well-child visits and vaccination visits.
Their results demonstrate how chatbots can be used innovatively to improve health disparities in a patient-centered manner:

Next, AllianceChicago partnered with Settlement Health and QliqSOFT, to improve personal, community, and public health through innovative collaboration, successfully executed through the RE-imagining Primary Care using Artificial Intelligence and Chatbots (REACH) project. REACH closes adult gaps in care and engages with patients who are overdue on preventive screenings and primary care services. The REACH project’s four objectives include:
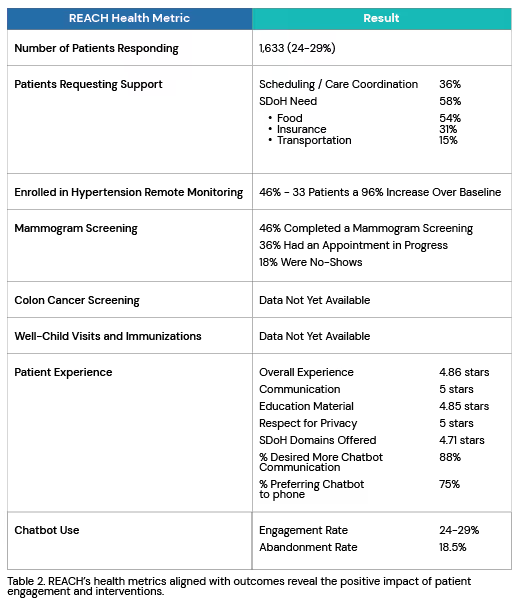
Multiple clinics have experienced challenges with systematizing SDoH screening within their workflow. Screening for SDoH at the point-of-care has presented barriers such as physical space, sensitivity of questions, and time and staffing needed to successfully screen and address needs. The REACH initiative demonstrated that chatbots could be successfully used to identify needs and redirect those needs to resources that could help address them. Their results are summarized below:
In addition to improvements in preventive care and capture of SDoH, proactive patient outreach provides the following benefits:
Chatbots are the ideal vehicle to engage patients outside of the walls of the clinic and nudge them to take proactive action to improve their health. QliqSOFT can help. Click here for a complimentary consultation to help you design and implement your patient outreach strategy.
