
CMS triples the weight of these measures because they directly reflect meaningful health outcomes for patients, such as preventing hospitalizations and effectively managing chronic diseases. This prioritization aligns with the CMS Triple Aim, focusing on improved patient experience, better population health, and reduced costs. By increasing the weight for these outcome-based measures, CMS incentivizes plans to implement proactive, evidence-based strategies that enhance care transitions and chronic condition management.
Triple weighting is used for measures that demonstrate real health improvement and support the overall CMS strategy of driving quality improvement and cost-effectiveness.
Three new measures are being added beginning with the 2026 Star Ratings: Kidney Health Evaluation for Patients with Diabetes, Improving or Maintaining Physical Health, and Improving or Maintaining Mental Health. Each of these measures has a 1x weighting for 2026, which increases to a 3x rating in 2027. This reflects the shift from patient experience to outcome-based measures.
Kidney Health Evaluation for Patients with Diabetes
For 2026, this becomes a new process measure in the CMS Star Ratings program. Both the Glomerular Filtration Rate (eGFR) test and a urine albumin-creatinine ratio (uACR) need to be assessed annually for individuals with diabetes. The eGFR test evaluates kidney function, while the uACR test assesses kidney damage. Together, they form a comprehensive kidney health evaluation that is essential for both the primary detection and ongoing monitoring of chronic kidney disease (CKD), as well as for the prevention and treatment of this condition.
Despite guideline recommendations, fewer than 50% of adults with diabetes receive annual kidney health evaluations, per the American Diabetes Association. Chronic kidney disease develops slowly, with a diabetic patient experiencing little to no symptoms until it is advanced. Approximately 1 in 3 adults with diabetes has CKD. Diabetes is the leading cause of end-stage kidney disease.
Patients with diabetes should see their physician every three to six months. 46% of Adults with Type 2 Diabetes don't see their physicians as often as recommended.
Here is where QliqSOFT’s proactive patient outreach can be of assistance. Organizations participating in value-based care can proactively reach out to their patients with diabetes to educate them on best practices for managing their condition, inform them that they are due for a visit, and make it easy for them to schedule appointments.
These organizations leverage QliqSOFT's population-level outreach and best practices to optimize patient participation, which maximizes the number of patients who engage with digital outreach. Our clients achieve response rates as high as 90%, which significantly impacts the number of attributed patients that physicians can evaluate and manage. Engaging these patients also has beneficial effects on completing other preventive care needs, such a verifying an eye exam was completed.
Improving or Maintaining Physical Health/Improving or Maintaining Mental Health
These two new measures place significant emphasis on longitudinal health and whole person care using Patient Reported Outcomes (PROs). It reflects the integration of the Health Outcomes Survey (HOS) measures into the Star Rating system. The Health Outcomes Survey (HOS) is a national survey program developed by CMS that measures the physical and mental health status and patient-reported outcomes of beneficiaries enrolled in Medicare Advantage (MA) plans.
The Improving or Maintaining Physical Health measure is made up of questions that speak to members’ ability to accomplish daily activities, like household chores, climbing stairs, and even bowling, without limitations from pain or otherwise limited mobility.
The Improving or Maintaining Mental Health measure is based on responses from the Health Outcomes Survey (HOS), where members self-report their mental health status—including feelings linked to depression, anxiety, loneliness, and isolation.
QliqSOFT’s Digital Patient Engagement Platform can help. Before a visit or on a schedule you determine, QliqSOFT can send surveys such as PHQ-9 depression scales and GAD-7 anxiety surveys to patients via text or email. As the patient completes and returns the survey, it is automatically uploaded into the EHR before the visit.
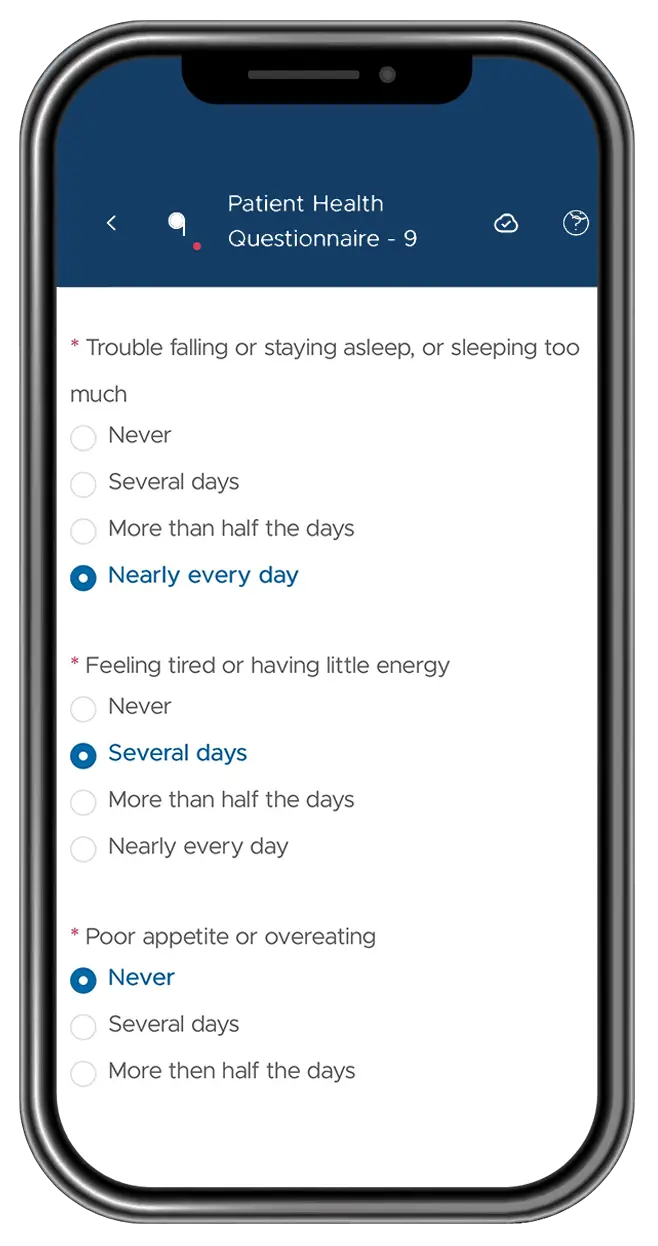
Staff also have access to a dynamic dashboard that shows the depression and anxiety levels of the practice’s population and patients, including the risk classification and score of each patient.

The benefit of capturing PHQ-9 and GAD-7 data before the visit includes efficiently screening for depression and anxiety symptoms, which helps clinicians identify patients’ mental health status early. This pre-visit data collection enables providers to review and discuss the results with patients from the start of the visit, allowing for more targeted and informed decision-making.
Previsit screening streamlines workflows by reducing the time required for symptom assessment during the appointment. Moreover, PHQ-9 and GAD-7 are validated, reliable tools with high sensitivity and negative predictive value, making them effective for early detection of common mental health conditions in primary care and other clinical settings. This supports routine mental health screening that is practical, easy to administer, and helps clinicians prioritize patients for further psychological evaluation or intervention as needed.
Preparing to deliver proactive patient outreach programs focused on the CMS Health Outcomes Survey (HOS) measures in 2026 lays the foundation for success, as these metrics will become triple weighted in 2027.
This preparation also allows plans to effectively allocate resources toward members who will benefit most from outreach, prioritize interventions for at-risk populations, and conduct mock surveys to identify and close gaps. The result is improved member experience, stronger health outcomes, and a competitive advantage in CMS quality performance programs as the weighting of these measures triples in 2027. Will you be ready?
In summary, early focus on these proactive outreach efforts aligns with the 2026 CMS HOS measures, helping health plans maximize their Star Ratings, enhance member health, and build readiness for the increased impact of these outcome metrics in 2027.
